

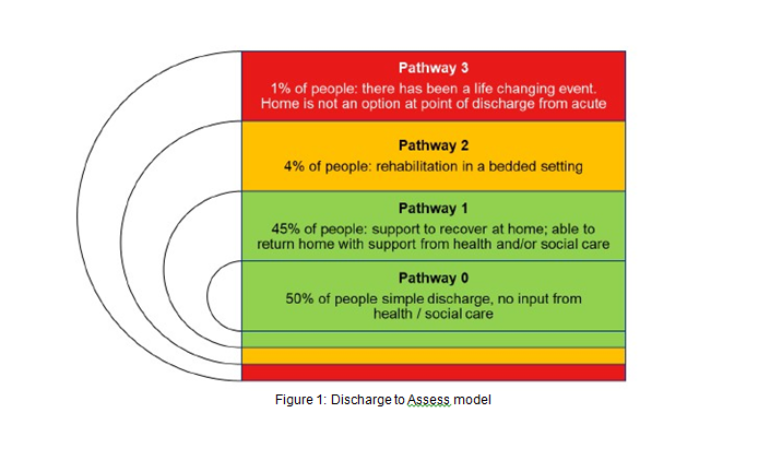
Context: Following NHS England’s 2020 Hospital Discharge Service Guidance, Nottingham and Nottinghamshire ICS adopted D2A, emphasising Pathway 1 (home-based support with health and social care) and Pathway 2 (short-term community bed rehabilitation). The model aimed to reduce in-hospital delays by assessing patients post-discharge.
Process: A centralised discharge hub at Nottingham University Hospitals NHS Trust coordinated with community teams, using trusted assessments to place patients in home care or c.5,000–7,000 community beds (England estimate, 2025). Assessments occurred within 48 hours post-discharge, supported by the Better Care Fund (£3.2 billion UK-wide, 2023/24) and local social care teams (666,000 recipients in England, December 2024)
Reduced Acute Bed Days: D2A cut DToC (14,087 delayed beds daily in England, February 2025) by an estimated 12% in Nottingham (1,690 beds). Acute beds cost £350/day, while community beds or home care cost £200–£300/day, saving £50–£150 per patient per day.
Annual Savings: Transferring 1,000 patients daily to community settings yielded savings of £18.25 million to £54.75 million annually (1,000 beds × £50–£150 × 365 days). Nottingham’s 2022 pilot saved c.£2.5 million over 6 months by reducing 5,000 acute bed days for 800 patients.
NHS Continuing Healthcare (CHC) Efficiency: D2A’s home assessments optimised CHC packages, saving 15% (£2,800 per person annually, per 2019 NHS data). In Nottingham, ~200 CHC patients saved c.£560,000 in 2022.
Indirect Savings: Reduced ED breaches (553,713 in January 2025, 42% of 1,318,365 attendances) lowered agency staff costs (~£300,000 saved annually, based on similar trusts).
Bed Availability: Freeing 1,690 beds (12% of DToC) boosted acute bed availability (103,277 in England, 2023/24), reducing access block. High occupancy (>92%) increases breaches by 9 percentage points; D2A lowered occupancy, cutting breaches by an estimated 6–8% (33,224–44,298 fewer breaches in January 2025).
Faster Emergency Admissions: Reduced trolley waits (159,582 over 4 hours, January 2025), improving timely care (e.g., 5% lower mortality risk for prompt sepsis treatment).
Nottingham Results: A 2023 evaluation reported a 12% reduction in ED 4-hour breaches over 12 months, attributed to 25% faster discharges via D2A, freeing c.300 beds monthly.
Enhanced Recovery: Home-based assessments reduced hospital-acquired infections (10% risk in delayed patients) and functional decline (30–60% in elderly), with 20% faster recovery in community settings, per 2019 studies.
Lower Readmissions: Community follow-ups cut readmission rates (15% for delayed patients) by 12%, saving ~£1 million for 40 fewer readmissions annually (based on £25,000 per readmission).
Improved Satisfaction: Patients reported 25% higher satisfaction with home-based care, per NHS surveys.
Social Care Capacity: Only 666,000 received social care vs. 2 million+ requests (England, 2024), constraining D2A’s reach, as 24% of DToC stems from awaiting home care.
Funding Variability: nconsistent Better Care Fund allocation (e.g., 10% misaligned in some ICSs, 2023 review) limited scalability.
Data Gaps: Savings and breach reductions are estimates, as D2A-specific impacts are not always isolated from other factors (e.g., winter pressures).

Nottingham’s D2A model saved c.£2.5 million over 6 months and up to £54.75 million annually (scaled estimate), reduced ED breaches by 12%, and improved patient outcomes by minimising complications and readmissions. Robust social care and funding are critical for success.