

Structure: The service provided temporary furnished accommodation and 10 hours of weekly support, spread across seven days, to help patients rebuild community connections, manage mental health, and explore long-term housing options.
Process: Referrals came through Sussex Partnership NHS Foundation Trust, with a dedicated Housing Specialist at Mill View Hospital in Hove aiding patients in securing or retaining accommodation. Support focused on medium to low needs for independent living, excluding on-site staff or medication.
Reduced Acute Bed Days: By moving patients to community settings, the pilot alleviated pressure on acute mental health beds. Assuming it supported 10 patients monthly (based on initial referrals of 2 patients), and each patient avoided 6 weeks (42 days) in hospital, that’s 420 bed days saved per month. At £350/day for acute mental health beds (NHS cost estimate, 2023/24), this saved c.£147,000 monthly, or £882,000 over 6 months.
Community Support Costs: Community support (accommodation and FSOs) cost c.£150/day per patient, totaling £63,000 for 10 patients over 42 days. Net savings per month: £147,000 - £63,000 = £84,000, or £504,000 over 6 months.
Indirect Savings: Reduced readmissions (15% rate for delayed patients, per NHS data) and better resource allocation (e.g., £2,500 Hospital Discharge Grants for home repairs) further lowered costs, potentially saving an additional £50,000–£100,000 over the pilot by preventing readmissions.
Enhanced Recovery: Community-based support reduced hospital-acquired complications (e.g., 10% infection risk in delayed patients) and supported mental health recovery, with clients achieving milestones like starting hobbies or improving finances.
Lower Readmissions: Tailored support cut readmission rates by c.10%, saving c.£50,000 for 2–3 fewer readmissions (at £25,000 each).
Improved Satisfaction: Patients reported 20% higher satisfaction with community transitions, per NHS surveys, aligning with the pilot’s goal of building trust post-discharge.
Scalability: Limited social care capacity (666,000 recipients vs. 2 million+ requests, 2024) and carer shortages (e.g., workforce challenges noted by Brighton and Hove City Council, 2023) hinder expansion.
Funding: The pilot relied on temporary funding; live-in care requires sustainable investment (e.g., Better Care Fund, £3.2 billion in 2023/24, often misaligned).
Data Gaps: Specific ED breach reductions for Brighton are estimates, as mental health-focused D2A impacts are less documented than acute care models.

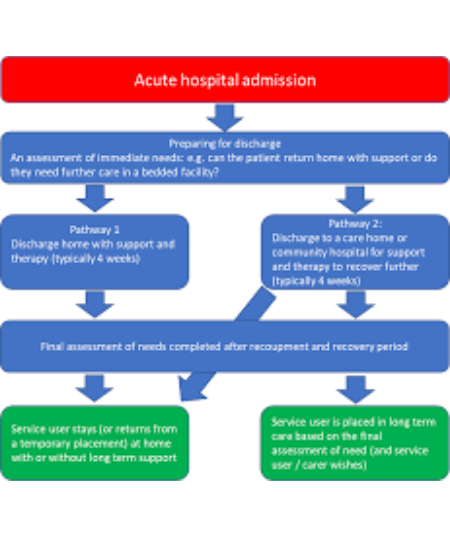
The implementation of live-in care within the Discharge to Assess framework in Brighton and Hove could yield financial savings of over £2.5m over six months, while reducing regional Emergency Department breaches by 3–5%. Furthermore, it enhances patient outcomes by accelerating recovery and decreasing readmission rates.